Challenges of Class within the Psychological Professions Part 2
By Ali Bryant, Expert by Experience, Member of PPN NW EbE Steering Group in conversation with Will Curvis and Katie Place
Exciting news on PPWeek24, new guidance on the Climate and ecological emergency from the Division of Clinical Psychology and more on the challenges of class from #ClassClinPsych collective members Will Curvis and Katie Place by Ali Bryant.
Listen to the blog here
This month part two of my conversation with Will Curvis and Katie Place on the challenges of class in selecting a career in the psychological professions and the benefits to recognising and owning class as part of your identity within the professions where services, the workforce and workforce retention are also topics under discussion.
But before that exciting news to share with you and a request to save the date for Psychological Professions Week 2024. PPWeek24 will take place between the 11th to the 15TH of November bringing you national and regionally delivered content. I for one can’t wait to be informed, enabled and influenced by what is on offer. More on the exciting programme to follow in September.
Close to my heart and interests is my involvement with the GTiCP Planetary Health subgroup and the work that has taken place in developing an important guidance document on planetary health for clinical psychology – this I know will also be of interest to a much, much wider audience. The guidance has just been published by the Division of Clinical Psychology part of the British Psychological Society (BPS) edited by Marc Williams and Ali Bennetts. Titled ‘Clinical psychology and planetary health: Changing course in a storm’ the guidance highlights the relevance to the profession of the climate and ecological emergency for their work and practice in supporting older adults, children, people with learning disabilities and health conditions and others to help the population adapt to CEE. The PPN NW EbE steering group cochair Joe Keaney is a contributor to the document and Joe and I are members of the planetary health subgroup. Currently access via DCP if you are a member at
Also in September the newly appointed Programme Manager for the Psychological Professions Network NW Phil Gooden will be the focus of the blog so watch this space to find out more about Phil and his hopes and aspirations for the PPN NW and more!!
But for now introducing or reacquainting you with Will Curvis and Katie Place from #ClassClinPsych Collective in a conversation continued from the July blog starting off with Will who left a question for us to consider- (link to part 1) https://ppn.nhs.uk/north-west/our-work/blog/item/challenges-of-class-within-the-psychological-professions-part-1
Will -Our trainees go out and learn about local communities and organisations. I really value that, and trainees get a lot out of it in their placements. But the gap is trainees qualify and then work in systems that are established and maybe disconnected. I've worked in services where you say, we could do this, but the response is there's no time, money, or resources. That is one of the big challenges for recruitment and retention in in clinical psychology, and it's not something we really talk about enough. If we can't keep staff in the NHS, in public services, then what's the point?
Katie-People struggle too working in services that feel very narrow in their scope or because they feel like they can't offer the kind of service that they want to offer. Sometimes it's as simple as why are we discharging a service user who missed two appointments, but no one is asking them why? Or if we did this, we might be able to engage them more. We need meaningful change on a bigger scale or we're going to have a profession who are burnt out because they don't feel like they can do what they need to do or address the needs of people in more marginalised communities.
Ali- Have you looked at the NHS benchmarking network’s Psychological Professions Workforce Census as it feeds into this conversation?
Will- Really interesting reading Ali which left me thinking that we need massive systemic change for the professions. It’s such a young group of people and a lot of shifting, people are staying on average about three years in roles. We also need systemic change to encourage people with better working conditions and better understanding of the career trajectory of clinical psychology as all health and care becomes more psychologically informed, and that's going to open up a lot of doors as more specialities start to take on psychologists.
Ali- We also have a population that's ageing, issues of multiple long term health conditions and we know social determinants of health is a key driver in MLTC’s and mental health. As clinical psychology becomes more embedded within the health space more of those conversations re #ClassClinPsych collective are going to be required so the population who have been disadvantaged get access to psychological professionals who have that blend of shared knowledge and background to support them.
Will- I think as a profession our strength should be grounded in helping us understand someone's experience and class is a massive part of that. There are so many professions where that isn't considered and ought to be. We can offer something more in depth in considering class, a more nuanced understanding of individual experience and collective experience. If we're not thinking about that in the context of the work we're doing, we're missing an opportunity to be meaningfully involved in promoting positive change.
Ali- I guess from my service user perspective If you have somebody in talking therapies and they're given 8 sessions, but they haven't got the money to get on the bus or they're having a really bad mental health day, a crisis, they haven't been able to eat, they've got to go to the food bank then the service user has got to make a choice. Missing a session may not be a priority that day but they are penalised by a system that's meant to be supporting them by depriving them of future therapy. That makes me just feel so upset. Potentially if someone in need had been able to attend they would have engaged but now at the point of care that door has been closed on them.
Katie- This is something that I've been really interested in. What are the factors that influence working class adults engaging in psychological therapies. Some of the things that you've just mentioned Ali came up, supporting an individual’s basic needs and staying alive can be more urgent than attending therapy. Getting to appointments, location of services are they accessible? Also beliefs are a barrier to engage in therapy, like they're not going to be able to address my problem. My problem is that I don't have a suitable house to live in or I don't believe that I deserve help as other people are worse off than me, so I won't engage because someone else needs the appointment more.
The service I worked in collected this data but most services don't. Much of the research was not specific to being working class so teasing out the data was not straightforward. I thought this focus would be on other people's research radar because working in services, I see these issues all the time.
Will- This issue gets broader and broader the more you think about it. When I qualified, I worked in some of the most deprived areas in Liverpool but my clinic was predominantly middle-class people. It's really hard to pin down but some of those areas have on average, lower reading ages because of social factors. We looked at the average reading age across those communities and one area had the lowest reading age in the country. Consider the implications in reading the letters that the hospital sends out for appointments with a massive gap between the contents and average reading age. With a potential lower reading age, it's no wonder people miss appointments beyond considerations of bus fare, time off work, childcare and day appointments Monday to Friday. Services don't really offer flexibility of when and where and how.
Ali- Also for people who are digitally impoverished with no broadband, or computer, they are already disadvantaged in a system that may have some flexibility for online appointments. Depending on their life circumstances and health and mental health conditions an online call might help support access. From what you have shared Will the way that information is presented needs to be looked at with different ways of presenting information ensuring equity in the language used in terms of reading age and access.
Will- The area where you live maps your trajectory for life. Some issues are elsewhere in systems and pathways. I worked previously in deprived areas, but they weren't who you saw in your clinic because most people referred via the GP. A GP is the gatekeeper to a service, the sense of what someone tells them is informed by their GP perspective. If a patient articulates things in a certain way, you're more likely to get a referral onwards. I think it's really hard to consider unconscious bias being embedded at that level. Layer upon layer of barriers to access. We're so used to working in certain models and systems that it completely impacts people's ability or services ability to think flexibly about what does this Community need. For example in terms of suicidality, alcohol, anger, big social issues, are we as psychological professionals involved in places where working class younger or older men go?
Ali- All of those, concerns really speak to me. Threaded through this conversation Will and Katie are opportunities and missed opportunities when the correct data isn't being collected because those people who ought to be there as service users aren't there. So any data is already skewed before it's been analysed.
Will- I can share an example of how perceptions about status affect interactions. I went to my GP with nonspecific symptoms which I researched online. The GP’s response was, are you a medical professional? I explained what I do for a living and he said I can hear that so we had a conversation as equals. If I hadn't been able to articulate my symptoms then I am uncertain I would have had the same outcome. Assumptions and negative narratives develop which stigmatise predominantly around class. Someone who is well spoken and articulate is treated differently than someone who can’t. The data's being missed as people are not getting the same access or opportunities because of an assumption. It’s the questions not asked in those conversations. Do you have a mobile phone to be contacted? Can you eat tonight? Its questioning yourself as a practitioner if you are working in a deprived area and the people you mainly see are middle class? As I mentioned trainees at Lancaster learn what they can about the community it breaks down barriers, supporting service users the people you work with on placement maybe a cue there for GP’s?
Ali- That knowledge is on a practical level going to be equally as valuable to service users as the therapeutic alliance. When the door closes on you until the next session or GP visit it’s knowing there is somewhere for you to turn to for the support you, your family or children need.
Katie-Getting to know the community you're serving is essential. Everyone in my cohort, came from different areas. We're all working in communities that are not communities we're familiar with so must invest time to do that research when moving roles particularly if the service we are joining has few community connections.
Ali- Thanks Katie. This aspect of the role is so important to consider around social determinants of health, health equity and socio-economic status and class in becoming a bridge to access for service users.
Katie- I think honest conversations are also required as psychological professionals as to, why people leaving are leaving the professions? A publicly funded healthcare system should, at its heart be driven by the needs of communities and the needs of the public. So why are people struggling to feel like they can do meaningful work in a lot of NHS services? Some services do really good work, are good at retaining staff and looking after people and in my own role I'm looked after engaged in innovative work connecting with my values.
Ali- From my perspective, change is required at a systemic level to have those conversations early around class and socio-economic factors to open up those doors to opportunity for people to join the psychological professions, including clinical psychology. But I guess, because of my own experience of socioeconomic disadvantage how do I from a service user stance outside of the profession get those conversations out there and talked about?
Will- It sounds like you're raising that awareness in publishing this for the PPN NW blog and I hope it's connected with where you're coming from and thank you for opening up the conversation. #ClassClinPsych are a tiny self-identified organisation and not connected to any bigger group, likeminded volunteers coming together, no bureaucracy, no red tape, we're not accountable to anyone so within reason speak to our values and concerns about class. We're a bunch of people who have a social media account. We don't have the reach of PPN/BPS yet in what we're trying to do so for now it’s about for now building those connections including a joint enterprise with the ACP putting together some guidance. We are passionate about having these conversations and I can recommend an interesting read the Class Ceiling – Why it pays to be privileged, it’s not specifically about the psychological professions, but it’s about all the professions and systemic barriers with regard to class, inclusion and diversity. I'm probably single handedly responsible for them having an uptick in sales because I recommend it to everyone.
Ali- Will, and Katie thank you both so much for giving your time to contribute to the blog and for a rich discussion which has resonated with me and I am certain will with everyone who reads it whether a psychological professional or service user to consider maybe for the first time the impact of class on individual identity, the professions, service users and services and barriers to access.
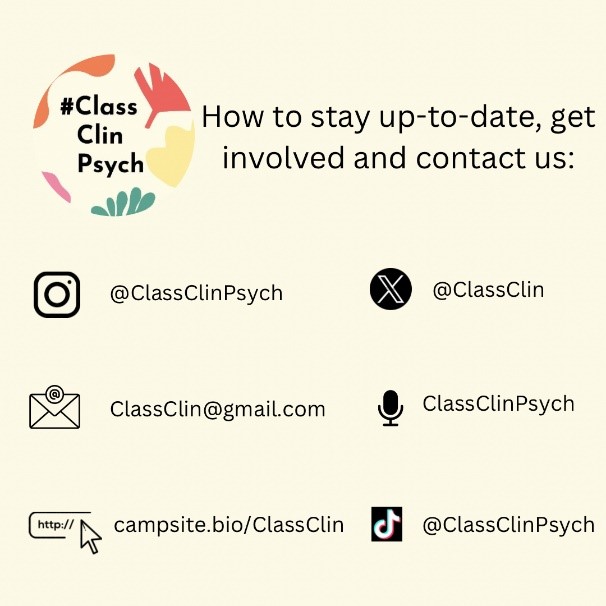
To find out more about #ClassClinPsych please follow
The Class Ceiling-Why it pays to be privileged by Sam Freidman and Daniel Laurison
Policy Press ISBN 978-1447336105
If you are not yet a member of the Psychological Professions Network, please join us and receive a PPN NW newsletter to inform you about what is happening in our region:
https://ppn.nhs.uk/membership/why-join-us
If we, at the PPN NW EBE steering group, can support you or your training courses, or offer any advice, please get in touch:
Until September please take the best care of yourselves,
Ali Bryant PPN NW EbE steering group.
